Taste, Nutrition, Diet and Recipes
Taste:
- One of the five senses, partners with the less direct sense of smell. There are four types of taste -sweet, bitter, sour and salt; and the recent addition of fifth – “umami” = savouriness
- Smell, texture and temperature are all important to taste. Flavour is also influenced by taste, touch, sight, pain and smell
Factors affecting taste:
- Taste cells are present on the tongue, upper palate, throat and oesophagus. Stomach receptors send messages to the brain about taste via the vagus nerve
- Chemotherapy, certain medications, hormones, upper gastrointestinal surgery and zinc deficiency can influence taste perception. Chemotherapy can damage the oral cavity leading to mucositis (inflammation of the lining) with ulcers and sores, infections, and salivary gland dysfunction. Cisplatin a chemotherapy drug frequently used to treat upper gastrointestinal cancers is known to affect taste.
- Roux-en-Y reconstruction can cause taste disturbance and also lead to aversion to meats and is associated with increased nausea and vomiting. Often there is also a decrease in taste perception; 45% patients with upper gastrointestinal resections suffer taste deficit. Full recovery usually occurs within 6 months in 67% of cases. Gastric reflux can impair taste perception.
- Zinc partly responsible for repair and production of taste buds. Approx 50% of drug-related taste disorders are caused by zinc deficiency as many medication bind to zinc preventing it from functioning properly
- Radiotherapy also affects the salivary glands. Saliva interacts and protects the taste receptors in the mouth.
- Tips for combating dry mouth: regular oral hygiene, mouthwashes, mints, sour sweets, sugar free gum, artificial saliva, crystallised ginger
Managing altered taste:
- Try new foods and cuisines e.g. Thai, Chinese, Mexican
- Flavour foods with herbs and spices e.g. fresh mint, basil, parsley, ginger, cinnamon. Add lemon juice to food as a marinade or dressing, try adding a few drops or a slice to your water.
- Refreshing drinks e.g. lemonade, ginger beer, herbal teas
- Cold foods with blander flavour and less smell can appeal especially to those suffering from nausea, taste aversions, sore mouths poor appetites e.g. potato salad, cold cuts, quiche
- Avoid metallic cutlery if you are suffering from metallic taste.
- Take plenty of fresh air and ensure your room is well ventilated.
- Distraction techniques (eg taking occasional bites whilst watching TV) and trying finger foods e.g. crisps/tortillas and dips, nuts, cocktail sausages
- Small plates with colourful presentation
- Do not worry about eating a “meal” initially, if you want to have biscuits for breakfast, jam doughnuts for lunch and cereal and toast for dinner it’s a start!
- Regular mouth hygiene is important
Nutrition:
- Pre-treatment (before chemotherapy/radiotherapy/surgery). Now is the time to build yourself up. Enjoy all your favourite foods and indulge. (but keep alcohol in moderation). Exercise is also encouraged at his stage to help you build stronger muscles and improve the health of your heart and lungs. Any weight you can put on now will be an advantage to you later regardless of your current size.
- Although some people sail through the chemotherapy others may not, and research has found that heavier people experience lesser side effects and have fewer breaks in treatment and are therefore able to receive a greater dose as well.
- Radiotherapy is very likely to make swallowing difficult, especially come your second week of treatment right up until 2 weeks after your treatment has finished; therefore any extra weight you can gain in preparation for this will put you in a greater position.
- The treatment that has the greatest effect on weight is surgery. You will usually have approximately 6 weeks after the end of your last chemotherapy cycle before your surgery is carried out. This is a good opportunity to try and increase your weight and fitness.
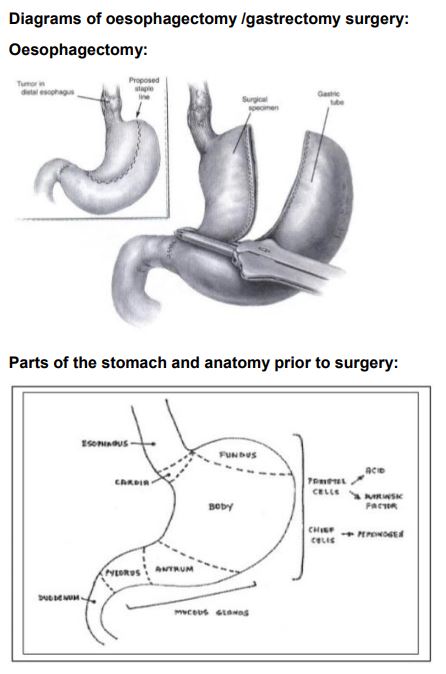
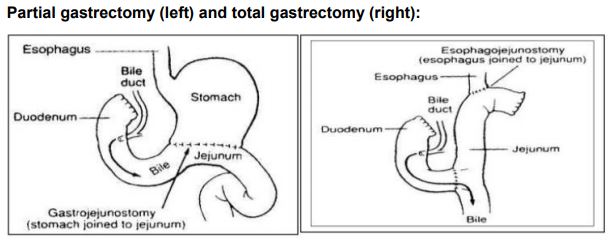
Post-surgery: this is a difficult time for most, especially for the first 6 weeks, with a considerable improvement at 6 months. Full recovery can take up to a year or more. Age plays a large factor, as does the extent and type of surgery. Total gastrectomy and oesophagectomy typically require longer recovery periods compared to subtotal gastrectomy or sleeve gastrectomy. The surgery has an impact on many areas your well-being:
- Appetite and intake is usually reduced after the surgery for some time due to many reasons: taste disturbance, nausea, previous anxieties and difficulties surrounding food, medications, fears of damaging the newly formed digestive tract, reduced capacity, fatigue and depression. It is important to monitor trends in portion sizes, variety, satisfaction, and confidence surrounding food (these should be increasing over time)
- It is important to receive regular follow-up during this time in order to ensure all barriers to eating and drinking are identified and addressed to allow for improvement.
- Holistic approaches: mood can decline after discharge from hospital, as there is less distracting activity compared to the ward and more time to reflect and worry. It is important to be as active as possible to regain your strength and avoid chest infections which can occur if you spend prolonged times lying or sitting. Also by being active and getting out of the house you are likely to feel better, more “normal” and develop more of an appetite. Do not attempt to do this alone though in the first instance; ensure you take a suitable friend or family member with you until you feel strong and confident enough.
- Digestive problems: it is common to experience diarrhoea for a few weeks after surgery, this should improve gradually, however it is important you discuss this with your dietitian, specialist nurse or doctor. It may be wise to ensure you have some Immodium or loperamide (which is the other name it is known as) at home. Ensure you are drinking well if you are having diarrhoea and eat small amounts regularly – do not avoid eating until the diarrhoea resolves. As your stools begin to form you may notice that they look oily in appearance, pale, floaty, fluffy; if this is the case you may be experiencing some difficulties digesting and absorbing fat (this is because of the reconstruction of your anatomy; it does not however happen to everyone). Reflux of acid or regurgitation of food can also occur after surgery; this usually improves with time, but please ensure your team is aware if this is a problem.
- Aims of treatment and support required vary: it is important to your team to know what is important to you in order to tailor your treatment accordingly. As a dietitian I am governed by what is important to you – provided it is not detrimental! Your aim may be to lose weight or to keep it steady or to try and gain a little; or it may not be important to you at all, you may be more focused on feeling well or being able to go out for a meal with your friends. It may be as basic as getting you eating something again. The amount of support everyone requires varies; I think it is important to establish how often and how the person would prefer to be supported e.g. face to face, over the phone, closer to home wherever possible.
Top Tips
- Eat small amounts regularly
- Keep liquids separate to solids (drinks and food separated by 30 mins intervals)
- Chew well and eat slowly
- Eating by the clock, rather than by appetite initially
- Avoid overfilling on fruits and vegetables until your eating is improved
Dumping Syndrome:
Early dumping syndrome occurs within 30 mins of eating – due to carbohydrates entering the digestive tract quickly and disturbing osmotic balance (ie concentration balance: fluids leaves the circulation system to even out with the concentration in the digestive system, leading to a decrease in blood pressure)
- Dizziness, faintness, palpitations, low blood pressure, cramping and diarrhoea
- Resting/lying down immediately after eating may help
Late dumping syndrome 2-3 hours after eating or if a meal is missed. This is due to poorly-timed insulin release for the amount of food entering the digestive system, affecting the insulin: sugar balance
- Feeling faint or sick or shaky
- Consuming a small amount of a sweet food may help
Recipes and Ideas:
- Delia Smith’s:
- Eggs Benedict
- Avocado and prawn/crab cocktail
- Jamie Oliver’s:
- Chicken liver parfait and brioche toast/baguette
- Chocolate fridge cake
- Nigella Lawson’s:
- Macaroni cheese
- Cherry cheesecake
- Mark’s and Spencer’s:
- Taramosalata and crisp bread/pitta bread
- Quiche
- Coleslaw
- Sainsbury’s
- Cauliflower cheese
- Taste the Difference Chicken Tikka Masala with Kasmiri pilau rice
- Luxury fish pie
- Porridge with Jersey milk and ground almonds
- Greek yoghurt with honey and nuts
- Cheesepuff straws
- Peanut butter with crackers
Based on a talk given by Stephanie Wakefield, Upper GI Dietitian, St Mary’s Hospital, Imperial College.
© The Oesophageal Patients Association


